Reducing The Hospital Readmission Rate Of Heart Failure
Faculty Mentor: Venkata Andukuri, MD, FHM
AIM: To reduce readmission rates of patients with heart failure (HF) by ten percent (based on the current rate of natural variation in our data) over the course of three months without affecting length of stay.
Introduction: Heart failure (HF) is a major cause of hospital readmissions and healthcare costs. HF patients have the highest rate of unexpected readmission of all diseases tracked by the Centers for Medicare and Medicaid Services (CMS), at 21.2% (1). HF prevalence is also projected to increase 46% from 2012 to 2030, with total costs rising from $30.7 billion to $69.7 billion by 2030 (2). Beyond the financial burden to patients and providers, a readmission increases the risk of additional hospitalizations and increases the risk of mortality, particularly within one month of discharge (3). The American Heart Association reports median 30-day readmission and mortality rates for HF of 21.9% and 11.6%, respectively (2). Interventions aimed at improving care and monitoring of patients during hospitalization and the first month after discharge could reduce both 30-day HF readmissions and mortality.
Studies and Results: For the baseline period from January through December 2018, Catholic Health Initiatives (CHI) Health Creighton University Medical Center - Bergan Mercy observed an 18.9% rate of 30-day readmission for patients with HF. The observed to expected readmission ratio was 1.35, indicating excess readmissions, a criterion for financial penalties through the CMS Hospital Readmissions Reduction Program. For the baseline data, there were 80 HF readmissions that occurred within 30 days. The HF-specific readmission rate was 42.5%, accounting for 6.8% of total hospital readmissions. The most commonly listed causes of readmission for patients discharged with HF were sepsis (18%) and nonadherence to medication regimen or dietary recommendations (16%). 45% of all HF readmissions occurred within one week of discharge from primary admission. 47 of the 80 patients (59%) received follow-up with the cardiology clinic or their primary care physician within 7 days of discharge. Another 20 patients (25%) received follow-up in 8-30 days, but 13 patients (16%) were not scheduled for a follow-up appointment. 21 of the 80 patients were discharged on the weekend. Of these 21, follow-up appointments within 7 days were not made for 13, or 62% of all HF patients discharged on the weekend.
From December 2018 through January 2019, all patients admitted with HF were offered to be interviewed by medical students during their hospital stay to learn more about how they understood and managed their HF and the barriers affecting their care. 40 total patients consented to the interview. 9 patients (22.5%) reported having run out of their HF medications at least once. 29 patients (72.5%) reported having a scale at home, but only 11 (27.5%) reported measuring their weight daily. 10 patients (25%) were not aware of any relation between their diet and HF, 9 (22.5%) reported not monitoring the amount of salt in their diet, and 16 (40%) reported not following any fluid restriction recommendations. Figure 1 below depicts the proportion of patients who reported being able to follow their medication and lifestyle recommendations.
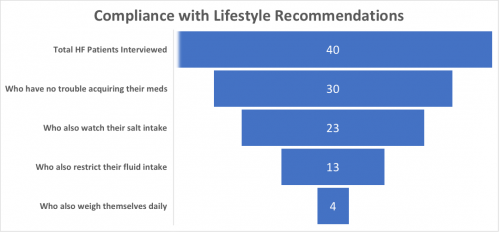
Figure 1: Funnel chart depicting the number of patients interviewed who reported following lifestyle recommendations for heart failure.
Significance of Results: All patients discharged during a weekday had a follow-up appointment scheduled by the time of discharge, while 62% of those discharged on the weekend did not have a follow-up appointment scheduled. The low rate of scheduled follow-ups for patients discharged on the weekend made it one of the most common factors contributing to readmissions, behind only sepsis, as depicted below in Figure 2. As early follow-up has been shown to reduce rates of readmission and mortality (4,5,6), weekend discharge is a promising target to improve care for our patients with HF.
The results of qualitative interview data showed rates of noncompliance with medication regimen and dietary recommendations similar to those found in the quantitative chart review. The qualitative interview data showed various reasons for noncompliance, including: cost of medications, transportation difficulties, a medication shortage at the pharmacy, underestimation of the importance of diet changes or weight, or not knowing/understanding their recommendations. Given that only 59% of all HF patients in the study have a follow-up appointment within one week of discharge, early and regular patient follow up can allow for improved discussion and monitoring of lifestyle changes, optimization of medications, and a more immediate response to difficulty with access to medications.
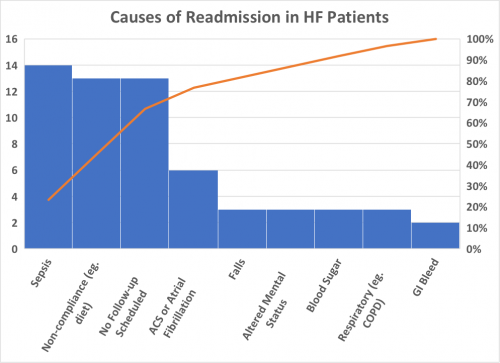
Figure 2: Pareto chart depicting the most common causes of 30-day readmission for patients with HF from our data.
Future Directions: Many primary care offices, and the CHI cardiology clinics, are closed on weekends, so it is not always possible for patients discharged on weekends to have an appointment scheduled by the time of discharge. In the coming months, I hope to introduce an intervention facilitating direct notification each Monday morning to CHI scheduling staff with the HF patients discharged that past weekend and require early follow-up appointments. With the low rates of patient-reported understanding and compliance with recommendations, this is another possible avenue for future intervention. There is also a high rate of early readmission – 45% within one week of discharge – suggesting that discharge processes deserve further study.




























































