Student Hospitalist Scholar Grant: Defining Existing Practices To Support The Sleep Of Hospitalized Patients - A Mixed-Methods Study Of Top-Ranked Hospitals
Faculty Mentor: Dr. Nicola Orlov, MD, MPH, Assistant Professor of Pediatrics, University of Chicago Medicine
This past summer, I learned what top-ranked hospitals are doing to improve inpatient sleep. The specific aims of the project were two-fold. First, we elucidated existing practices to improve inpatient sleep at highly-ranked hospitals. An anonymous, quantitative survey was created based on the current literature and distributed to the Section and Division Chiefs of Hospital Medicine at the 2020 US News and World Report (USNWR) Honor Roll Best Hospitals (20 adult and 10 pediatric institutions) to understand the policies in place to improve sleep in their hospitalized patients. Second, we elucidated the prevailing attitudes and best strategies to improve inpatient sleep at highly-ranked hospitals. A qualitative interview based on the 4D cycle of appreciative inquiry1 was created and the same population was invited to participate. These structured interviews allowed hospitalist leaders to both discuss the progress their institution has made to promote inpatient sleep and share their perspectives on ways to improve future sleep-friendly standards at their hospital and across the nation.
Our total survey response rate was 77% (n=23/30; pediatric response rate = 80%, n=8/10; adult response rate = 75%, n=15/20). While 96% of the respondents (n=22) rated sleep in hospitalized patients as important, only 44% (n=10) said that they were satisfied with their institution’s efforts to improve patient sleep. Furthermore, while 91% (n=21) of hospitalist leaders rate sleep equity as important, only one institution (4%) has practices in place to address this disparity. Less than half (n=11) of surveyed institutions are actively working to improve sleep; 52% (n=12) of institutions reported having no-sleep friendly practices in place. Across the 11 institutions with sleep-friendly practices in place, the most common sleep-friendly practices included reducing overnight vital sign monitoring (43%, n=10), decreasing ambient light in the wards (43%, n=10), adjusting lab and medication schedules (35%, n=8), and implementing quiet hours (30%, n=7) (Figure 1).
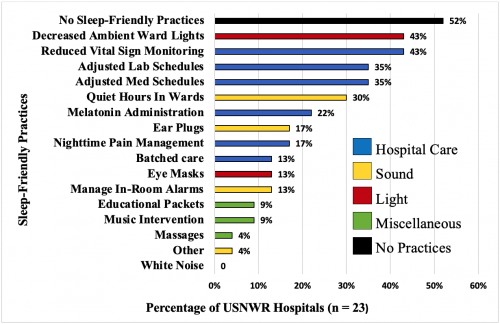
Figure 1. Reported Sleep-Friendly Hospital Practices at USNWR Honor Roll Hospitals, n=23. "Other" practice listed was to rubberize floors to reduce noise.
Twenty-seven percent (n = 8/30; pediatric interviews = 3/10, 30%; adult interviews = 5/20, 25%) of USNWR section chiefs participated in our interviews. After analyzing the sessions, four overarching themes emerged. The major themes were “Universal Culture/Shared Understanding,” “Environmental Changes,” “Hospital Practices,” and “External Incentives.” Environmental changes (like sound reduction) and hospital practices were also featured in the previous literature and our survey results. Examples of successful modifiable practices associated with these themes were to have universal times to dim lights and reduce sound, and to group tasks in order to reduce the number of room entrances. Notable barriers included having high-patient volumes and using medical devices (like intravenous poles and alarms) that create noise in patient rooms instead of alerting hospital staff directly.
Having a hospital sleep-friendly culture and external drivers to improve sleep were unique interview findings. Many section chiefs reported that having “buy-in” or any unified effort made programs successful and/or helped lead to future success. They also described how the culture dictates how the care team practices, where “people do the same things they would do for the same [disruptive practices] they would do for the sicker patient for the less sick patient,” even if it is unnecessary or hinders sleep. The section chiefs expressed the need to have external incentives to motivate a change in culture, where some current efforts were only possible because external grant funding, hospital ratings, or outside expert support incentivized them (Table 1).
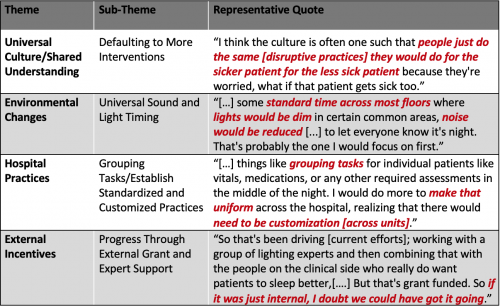
Table 1. Qualitative Descriptions of Existing and Potential Sleep-Friendly Practices, n=8.
This is the first multicenter study to identify the existing practices used by highly-ranked hospitals to support the sleep of hospitalized patients. The results demonstrate the well-recognized importance of inpatient sleep, while simultaneously identifying a need to improve current practices. Our findings are alarming considering the significant adverse effects associated with sleep disruption in hospitalized patients. The structured interviews contextualized some of the reasons why progress has been slow in the past, but also suggest avenues for hospitalists to improve moving forward.
Our team hopes to perform a similar study with highly-rated institutions on the Hospital Consumer Assessment of Healthcare Providers and Systems “quiet at night” survey question. Since they have received favorable scores from patients regarding their sleep practices, they may be positive deviants in patient sleep promotion among US hospitals. One such institution’s innovation officer reported decreased rates of Clostridium difficile among other benefits from actively and effectively improving hospitalized patient sleep. It will be important to champion these institutions that have had success and to develop a standardized set of sleep-friendly best practices.
Reference
1. Trajkovski S, Schmied V, Vickers M, Jackson D. Implementing the 4D cycle of appreciative inquiry in health care: a methodological review. J Adv Nurs. 2013;69(6):1224-1234.






























































