SHM Student Hospitalist Scholar Program - Final Project Report
Association between Sleep Quality, Health Literacy, and Patient Outcomes in Hospitalized Diabetic Patients
Author: Ojas Deshpande, MS at the California University of Science and Medicine
Project Mentors: Dr. Vineet Arora MD, MAPP & Dr. Valerie Press MD, MPH, FACP, FAAP, SFHM, ATSF
Research is a crucial component of medicine. I had the honor of participating in a clinical research initiative at a world-renowned institution wherein the faculty exemplify a genuinely collaborative spirit. Within the scope of this research initiative, I worked on a retrospective project surrounding diabetic inpatients, their sleep, and health literacy.Project-specific aims:
Sleep is a vital body process, dictated by psychosocial, biological, and evolutionary phenomena we are still learning about in greater detail. The advent of sleep actigraphy has enabled us to quantify parameters such as sleep latency and efficiency with objectivity and portability. Subjective sleep data using validated tools is also an excellent form of screening to appreciate sleep's impacts on biological and psychological parameters.Acute and chronically poor-quality sleep have been shown to adversely affect diabetic patient outcomes more so than non-diabetic patients, through proposed mechanisms including cortisol-mediated hyperglycemia1. Since diabetic inpatients are at increased risk of poor outcomes, our team sought to better characterize the association between sleep, outcomes (including readmission rate and risk), and health literacy within this population.
Health literacy as a determinant of health may also influence outcomes such as length of stay (LOS)2 and readmission risk3. As a secondary aim, we sought to identify associations between objective sleep data and outcomes while stratifying subjects by health literacy. Finally, some studies have associated low health literacy with overall lower perceived self-health status2. Thus, we also sought to determine the associations between subjective sleep measures such as the Pittsburg sleep quality index (PSQI) and health literacy to see if low health literacy itself is associated with poorer sleep quality.
Project design:
We followed a cohort study design of diabetic inpatients admitted or transferred to the general medicine service at the University of Chicago. Participants were diabetic adults (with confirmed medical diagnosis of diabetes in the medical record) aged 50 and older living in the community before admission. Exclusion criteria included observation status, age under 18 years, non-English speaking, patients with previously diagnosed sleep disorders, and cognitive impairment (Mini-Mental State Examination telephone version score <17). Actigraphy measured hospital sleep duration and efficiency, while subjective sleep indices were measured using the PSQI and Epworth sleepiness scale. Health literacy was measured using the Brief Health Literacy Screen (BHLS).Data is currently being analyzed using the SPSS analysis platform. An ANOVA analysis examined the relationship between sleep quality (subjective and objective) and literacy to contrast each sleep quality measure's relationship with health literacy. Chi-squared and 2-tailed t-tests compared categorical and continuous variables.
Preliminary results:
Inclusion criteria were met by 512 patients who were evaluated for the parameters discussed. The patient population had a diverse array of principal diagnoses. The most common included kidney disease (12.3%) and pancreatic disease (8.8%). In terms of health literacy, approximately 21% had inadequate health literacy as determined by the BHLS. Participants with low health literacy were more likely to be older (58% vs 36%; P = 0.02) and did not have a high school education (28% vs 15%; P = 0.011).When comparing sleep quality (a PSQI qualitative metric) and actual sleep efficiency, we performed a Kruskal-Wallis ANOVA using sleep quality perception as the independent variable. A significant association was not seen (H[4] = 2.13, p = 0.28).
When assessing the association between sleep quality perception and health literacy using chi-square testing, a significant association between health literacy as an independent variable and perceived sleep quality was found (p=0.038). However, no significant association between overall PSQI score and health literacy was observed using a Wilcoxon-Whitney test (U=10.8, p = 0.31). Logistic regression determined an association between sleep efficiency on total LOS (OR 0.78, 95% CI [0.71-0.84], p = 0.044).
Significance of results:
With the exciting association observed between health literacy and perceived sleep status, further analysis should assess the impacts of health literacy on individual components of the PSQI. Although no significant association between overall PSQI score and health literacy was observed, it is interesting to see an association between individual components which may be more sensitive or specific for patients with low health literacy.Finally, evaluating the effects of poor sleep on LOS, controlling for diabetic inpatients with low health literacy, revealed a significant association when poor sleep was the independent variable. Further analysis must appreciate the impact of stratifying by health literacy by comparing sleep efficiency and LOS in high health literacy inpatients. In collating this data with the literature, it is fascinating to see how psychosocial complications of low health literacy may impact patient recovery time (and thus LOS) or patient participation within this diabetic inpatient population. Low health literacy may thus exacerbate poor outcomes in diabetic inpatients, although further analysis must be conducted to adequately determine this. Moreover, the pathological impacts of poor sleep result in an increased cost burden on care systems, as shown in figure 1.
Future work:
Given the salient associations observed, a significant portion of the analysis must explore these observations through different lenses (both statistical and using other metrics within the dataset). For example, further investigation will examine associations between the Epworth sleepiness scale score and health literacy (and individual scale components). Moreover, a detailed analysis of sleep impacts for patients with low health literacy on diabetic inpatient readmission will be assessed using ROC analysis. I plan to continue exploring the many facets of health literacy, sleep, and their impacts on diabetic inpatient care through this analysis. Eventually, I hope these findings may supplement the integration of sleep interventions for at-risk diabetic patients in the wards!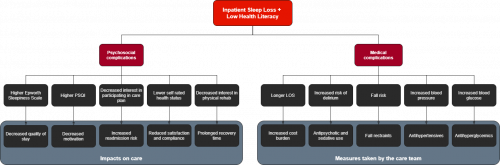
Figure 1: Flowchart depicting potential medical and psychosocial complications of low health literacy and inpatient sleep loss on patient care, based on findings from this project and the literature.
- Li, Mingzhen, Daiqing Li, Yunzhao Tang, Lingling Meng, Cuixiu Mao, Lirong Sun, Baocheng Chang, and Liming Chen. "Effect of diabetes sleep education for T2DM who sleep after midnight: a pilot study from China." Metabolic syndrome and related disorders 16, no. 1 (2018): 13-19.
- Jaffee, Ethan G., Vineet M. Arora, Madeleine I. Matthiesen, David O. Meltzer, and Valerie G. Press. "Health literacy and hospital length of stay: an inpatient cohort study." Journal of Hospital Medicine 12 (2017)
- Deshpande, Ojas A., John A. Tawfik, Aram A. Namavar, KimNgan P. Nguyen, Sitaram S. Vangala, Tahmineh Romero, Neil N. Parikh, and Erin P. Dowling. "A Prospective Observational Study Assessing the Impacts of Health Literacy and Psychosocial Determinants of Health on 30-day Readmission Risk." Journal of Patient Experience 9 (2022)




























































